Posts
40 Year old female eith urethral stricture under evaluation
- Get link
- X
- Other Apps
40 year old female WITH urethra stricture under evaluation CASE HISTORY A 40 year old female , house wife ,CAME from west bengal WITH CHEIF COMPLAINTS OF - dysuria decreased frequency of urination post void urinary retention and slow urine stream since 6 months burning micturition since 5 months dysperunia since 4 months loin and lower back pain since 1 month HISTORY OF PRESENTING ILLNESS - patient was apparently asymptomatic 6 month back then developed dysuria which was insidious in onset gradually progressive associated with burning micturation retention of urine and lower abdomen pain and distension the pain in abdomen gets relieved with medication and voiding urine burning micturition not associated with any fever cough nausea vomiting patient developed dysperunia 4 months back and pain in the flanks and lower back 1 month back no SIGNIFICANT PAST HISTORY , AND THEN CAME TO KIMS FOR FURTHER EVALUATION PAST HISTORY - n/k/c...
13 YEAR OLD BOY COMPLAINTS OF HIGH GRADE FEVER SINCE 4 DAYS
- Get link
- X
- Other Apps

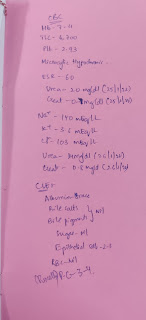
13 YEAR OLD BOY COMPLAINTS OF HIGH GRADE FEVER SINCE 4 DAYS A 13 year old school going boy complaints of - high grade fever since 4 days - vomitings since 4 days - giddiness ince 4 days - loose stools since 1 day Patient was apparently asymptomatic 4 days back then he developed fever associated with chillschills. Complaints of vomiting since 4 days- 2-3 episodes/day with food particles as content Loose stools- 5 episodes in the past one day No history of burning micturition, melena, rashes, bleeding gums, hematuria VITALS Temp- 98.8 F PR- 90 bpm BP- 100/60 mmHg RR- 18 cpm Spo2- 98% at RA GRBS- 118mg% GENERAL EXAMINATION Patient is conscious, coherent and cooperative. No signs of Pallor, Icterus, Cyanosis, Clubbing, Lymphadenopathy or Edema. SYSTEMIC EXAMINATION CVS: S1 S2 heard, no murmurs/thrills RS: BAE+, NVBS heard PA: Soft, non tender. Liver and Spleen not palpable. Bowel sounds heard. CNS: NFND PROVISIONAL DIAGNOSIS NS 1 + DENGUE INVESTIGATIONS Outside Repor...
55 Y /M WITH HEART FAILURE , ? COPD , BELOW KNEEAMPUTATION
- Get link
- X
- Other Apps

55 Y /M WITH HEART FAILURE , ? COPD , BELOW KNEEAMPUTATION 55 Y / M pt presented to casuality with c/o Blurring of vision since 1 year Decreased urine output since 2 months Pedal edema since 1 month SOB since 3 days Distended abdomen since 2 days Pt was apparently asymptomatic 10 yrs back , then he was diagnosed with DM type 2 , on has been using Glimi 2 mg tablets Pedal edema was gradually progressive SOB grade 4 was more during the night , PND There are no aggregating and relieving factors Pt is a k/c/o DM since 10 yrs , on Tab Glimi 2 mg HTN since 2 yrs , on T. Telma 40 mg Surgical history : Pt had below knee amputation 1 yr back , due to trauma to the left lower limb which developed cellulitis Pt is an occasional alcoholic since 30 years Chronic smoker since 20 years ( daily 1 pack of cigarette and 1 pack of beedi ) Medical h/o : Pt is on T Atorvastatin 10 mg T Pentoxif...
50 year old male on MHD
- Get link
- X
- Other Apps

A 50 year old male patient is on maintainance haemodialysis since 10 months. HOPI: patient was apparently asymtomatic 4yrs back and then developed shortness of breath (on and off), pedal oedema (pitting type).Later diagnosed as chronic renal failure and underwent dialysis twice weekly for about 10 months. 6 years back he met with an accident. His right leg got fractured and it took nearly 1 year to heal for which he used few medication continuosly for 1 year. PAST HISTORY: k/c/o HTN since 1 year. Not a K/C/O of DM, thyroid disorders, TB PERSONAL HISTORY:He follows a mixed diet. Appetite -Normal, Bladder movements-normal, Bowel movements-constipation since few weeks. Sleep- decreased.consumes alcohol regularly(90ml ) and stoped consuming1 year back. He is a farmer and stopped working since 1 year. FAMILY HISTORY: No significant family history. DRUG HISTORY: No known drug allegies and patient uses Nicardia 10 mg. General examination : patient is conscious ,coherrent, co operative a...